My final post on cracks (well, until the next one, lol)
When lecturing, I am often asked at what point would you save the tooth?
In other words, how deep can the crack go (and be visualized on 3D) and still proceed with endo/resto/saving the tooth.
This is a complex and interdisciplinary answer, but here we go….
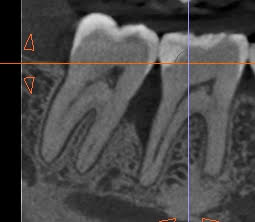
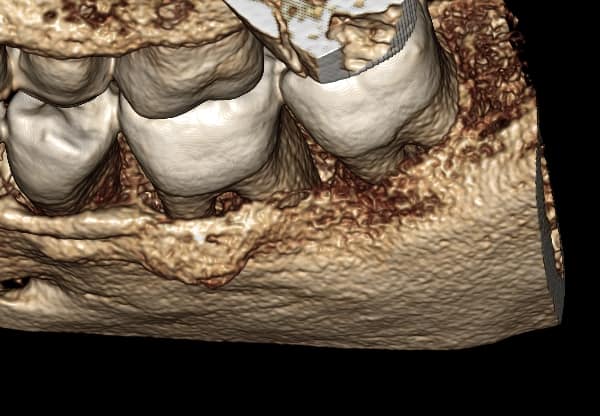
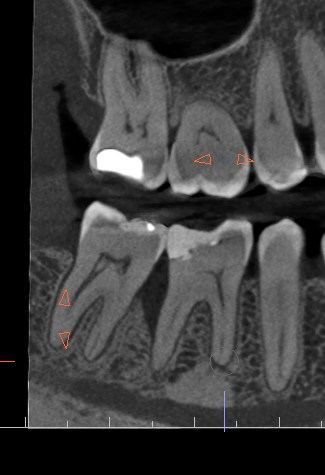
First and foremost, I start with my pulp testing. Sometimes there is a probing defect, sometimes there is not. Sometimes there is a bridge OVER the probing defect so the ppd will be inaccurate! So, then, next is CBCT/3DImaging, which brings things to light.
Important things to consider once you have probing & the rest of the PVTesting results together with the Clinical exam, the pt’s CC and their imaging: PA, BWs & 3D scan:
1) I am a endodontist – as a specialist, I defer and follow the lead of my quarterback, my RD, after a convo with the patient
2) In these cases, no matter the crack’s extent, I *must* and do connect with the pt’s general dentist, and if I can’t get them while the pt is in my office, I tell the pt that I will connect with their GD and then one of us will get back to the pt with the plan for the next steps either way
3) Oftentimes, the dentist decides that usually about 3 mms BELOW the crestal horizontal bone, the prognosis is poor, and recommends exo/implant.
The dentist usually then connects with the patient, or will ask me to relay this. This is generally *after* the consultation is well over, usually in the next few days. Obviously, if symptomatic and urgent, then conversations are attempted in real time when possible.
4) After that, a small subset of patients will still want to try to save the tooth, and that is fine too. If I had a cracked tooth, tbh, I would want to save it!
I – personally – don’t have enough follow-ups on these yet to have come to any conclusions re: what should be attempted to be saved, and what should not. However, I generally consider, “if it were my tooth, what would I do?” and often I would want to try to save the tooth, even if it means a borderline prognosis and knowing that I might only have the tooth for a few years. This convo also gets documented in the pt’s chart. There are a few articles on cracks in the literature. Usually, the long-term prognosis is dismal, most especially (imho) because we’re catching them too late.
The case below shares a patient with a very very deep angular defect. This could not be saved, and in this case, there was no conversation about saving; I advised extraction. IMHO, it would be a waste of everyone’s time and the pt’s resources to attempt further dentistry on this tooth.
The conversations we SHOULD be having however are the incipient cracks and smaller ppds that we encounter – esp during prophy visits with pts’ #hygienists !
My #protip is that we should be starting these conversations about 1) occlusal guards and 2) full coverage restorations – so as to avoid the propagation of these cracks.
I will share some cases that I think we should save in another post soon….